In the complex world of healthcare financing, the concept of Diagnosis-Related Group (DRG) mismatch emerges as a significant challenge for providers navigating the nuances of various payment systems. Understanding DRG mismatch and different payment versions is crucial for healthcare professionals and financial managers. This guide aims to provide a comprehensive overview of DRG mismatches, the implications of different payment versions, and tips for managing these complexities effectively.
What is DRG Mismatch?
DRG mismatch occurs when there is a discrepancy between the diagnosis recorded and the assigned DRG code, which may lead to improper reimbursement from insurers. This problem can arise due to clerical errors, improper coding practices, or differences in interpretation of clinical documentation.
The Impact of DRG Mismatch on Healthcare Providers
DRG mismatches can have financial implications for healthcare facilities, affecting their revenue cycle management. When reimbursement is tied to the accuracy of DRG coding, any mismatch can lead to underpayment or overpayment, complicating the billing process.
Common Causes of DRG Mismatch
- Poorly trained coding staff
- Incomplete medical documentation
- Changes in clinical guidelines
- Differences in payer requirements
Different Payment Versions: A Breakdown
The variety of payment systems in the United States healthcare sector can make it challenging for providers to maintain compliance with DRG coding. Here, we explore the major payment versions impacting DRG coding.
1. Medicare DRG Payment System
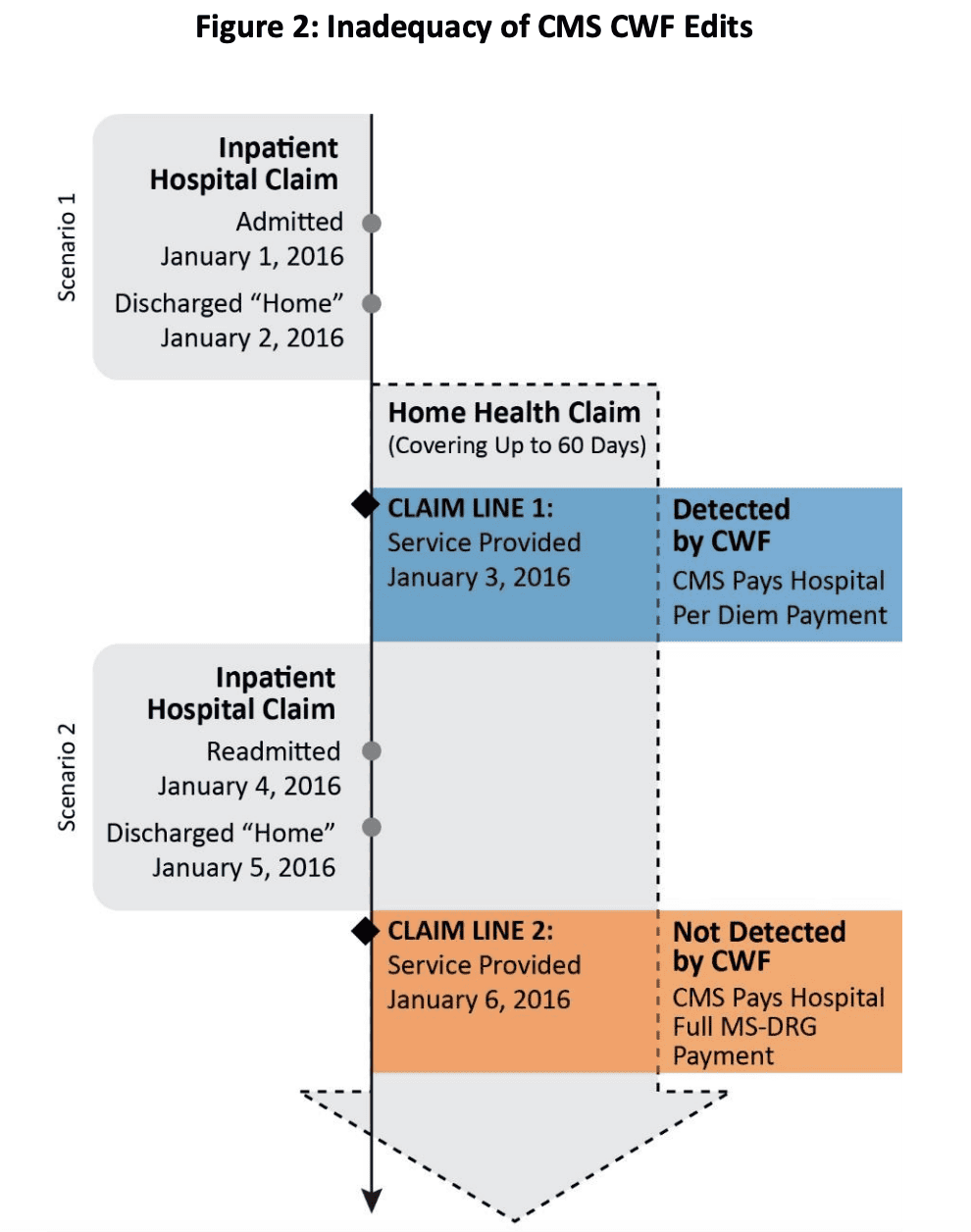
The Medicare DRG payment system is widely recognized as the benchmark, where the Centers for Medicare and Medicaid Services (CMS) assigns a payment rate to hospitals based on the DRGs.

Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Standardized payments | Complex coding requirements |
| Predictability in revenue cycle | Penalty for readmissions |
| Encourages efficient care delivery | Risk of insufficient reimbursement |
2. Medicaid DRG Payment System
Each state administers its DRG payment system under Medicaid, leading to significant variations in reimbursement amounts and processes.

State Variability and Its Effects
The variability among states can create confusion. For example, California employs a value-based purchasing model impacting DRG payments, while Texas has a different approach that may prioritize different factors.
3. Commercial Insurer DRG Payment Systems
Private insurers often develop their DRG payment methodologies, which can differ significantly from Medicare or Medicaid systems. This can lead to mismatches if providers aren’t aware of the specific conditions tied to these contracts.

Comparison of Commercial Insurers’ DRG Payment Systems
| Insurer | Payment Model | Key Features |
|---|---|---|
| Blue Cross Blue Shield | Fee-for-Service | Flexible reimbursement rates based on negotiated contracts |
| Aetna | Value-Based Care | Incentives for quality outcomes |
| UnitedHealthcare | Bundled Payments | Fixed payment for entire episodes of care |
Navigating DRG Mismatch: Strategies for Healthcare Providers
Given the challenges presented by DRG mismatch and varying payment versions, healthcare providers can adopt several strategies to improve accuracy and compliance.

1. Invest in Training and Education
Regular training sessions for coding staff can drastically reduce DRG mismatches. Familiarity with updates in coding guidelines, such as ICD-10 changes, is crucial.
2. Implement Robust Documentation Practices
Encouraging thorough medical documentation ensures that coding staff has all the information necessary to assign accurate DRG codes. This includes detailed notes on patient conditions and treatment plans.

3. Leverage Technology and Software Solutions
Utilizing advanced coding software can help reduce human error in DRG assignments. Many platforms now offer real-time coding assistance and feedback.
Recommended Coding Software Solutions
- 3M CodeFinder: Offers comprehensive coding support and analytics.
- Optum360: Provides a range of coding solutions, including DRG management tools.
- Nuance Dragon Medical: Speech recognition technology that improves documentation accuracy.

Pros and Cons of Different DRG Payment Methods
Understanding the pros and cons of various payment methods can help providers choose the best fit for their operations.
Medicare Advantage Plans
Medicare Advantage plans sometimes offer additional benefits compared to standard Medicare.
Pros
- Often include vision and dental coverage
- Fixed copays for services
Cons
- Network restrictions can limit provider choices
- May require prior authorization for certain services
Accountable Care Organizations (ACOs)
ACOs focus on providing coordinated care while sharing savings from reduced hospital admissions.
Pros
- Incentivizes preventive care
- Potential for shared savings
Cons
- Complex agreements and reporting requirements
- Risk of penalties for high spending
Conclusion: The Future of DRG Mismatch and Payment Systems
As we move forward, the healthcare landscape continues to evolve with changes in regulations, technology, and consumer expectations. Staying informed about DRG mismatches and payment systems is crucial for healthcare providers aiming to maximize revenue and ensure quality patient care.
FAQs About DRG Mismatch and Payment Versions
What causes a DRG mismatch?
A DRG mismatch typically arises from errors in coding, insufficient documentation, or misunderstandings of payer requirements. Training and better documentation practices can help mitigate these issues.
How can technology help with DRG coding?
Technology can streamline the coding process, reduce human errors, and provide real-time feedback on coding decisions, making it easier to maintain compliance with DRG guidelines.
What are the differences between Medicare and Medicaid DRG systems?
Medicare’s DRG system is standardized nationwide, while Medicaid systems vary by state, leading to different reimbursement rates and coding requirements.
Why is accurate DRG coding important?
Accurate DRG coding ensures that providers receive appropriate reimbursement for their services, which is crucial for maintaining profitability and offering high-quality care.
Are there penalties for DRG mismatches?
Yes, healthcare providers may face penalties for DRG mismatches, including financial repercussions from underpayments or potential audits from payers.